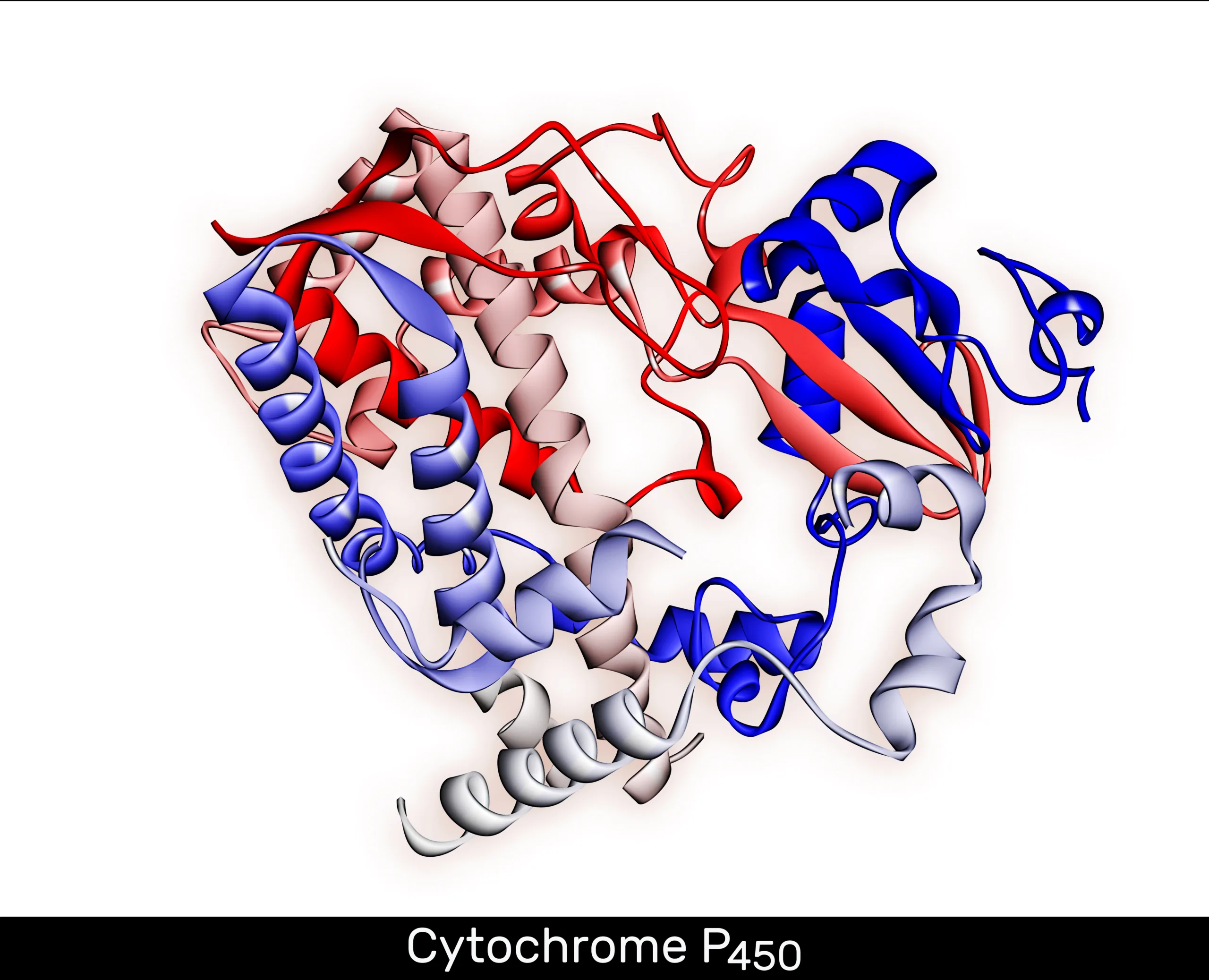
Cytochrome P450 Genotyping Panel Explained
Did you know that our unique genetic makeup can greatly influence how our bodies metabolize medications? It’s estimated that up to 70% of all drugs are metabolized by a group of enzymes called cytochrome P450 (CYP450).

Understanding how our genes interact with these essential enzymes is crucial for personalized medicine. This is where the cytochrome P450 genotyping panel comes into play. By analyzing specific genes involved in drug metabolism, this innovative genetic test can provide valuable insights into an individual’s risk of abnormal drug metabolism and guide personalized medication management.
Key Takeaways:
- Up to 70% of all drugs are metabolized by cytochrome P450 enzymes.
- The cytochrome P450 genotyping panel analyzes genes involved in drug metabolism to provide personalized pharmacogenomic insights.
- Understanding an individual’s cytochrome P450 genotype can optimize drug selection and dosing.
- The panel offers advantages in personalized medication management and can improve patient outcomes.
- Results from the panel help healthcare providers tailor treatment plans based on an individual’s genetic profile.
What is Pharmacogenomics?
Pharmacogenomics, also known as pharmacogenetics, is the study of how genes affect an individual’s response to medication. It involves analyzing genetic variations to determine how drugs are processed and metabolized by the body. By understanding how an individual’s genes influence drug metabolism, healthcare providers can tailor medication regimens to maximize effectiveness and minimize side effects. Pharmacogenomic testing, like the cytochrome P450 genotyping panel, plays a crucial role in personalized medicine testing.
Pharmacogenomics focuses on examining how an individual’s genetic makeup affects their response to different drugs. This branch of genetics provides valuable insights into drug metabolism and ensures personalized medication management. By analyzing genetic variations, such as single nucleotide polymorphisms (SNPs), it becomes possible to determine how a specific drug will be processed and utilized in an individual’s body.
The field of pharmacogenomics aims to identify genetic markers that can predict an individual’s response to specific medications. This information is crucial in tailoring treatment plans and optimizing medication regimens for individual patients. By utilizing pharmacogenomic testing, healthcare providers can select drugs that are more likely to be effective and minimize the risk of adverse reactions.
“Pharmacogenomics allows us to move away from a one-size-fits-all approach to medication management and towards personalized medicine that takes an individual’s genetic makeup into account.”
Understanding Genetic Testing in Pharmacogenomics
In pharmacogenomics, genetic testing plays a central role in determining an individual’s drug response. Genetic testing involves analyzing an individual’s DNA to identify specific variations or mutations in genes associated with drug metabolism. This information helps healthcare providers understand an individual’s unique drug metabolism patterns and tailor medication choices accordingly. Pharmacogenomic testing can provide insight into how a patient will metabolize certain drugs, allowing for better treatment planning and individualized care.
The process of genetic testing in pharmacogenomics typically involves collecting a DNA sample through various methods, such as a blood or saliva sample. The DNA is then analyzed for specific genetic variations using advanced laboratory techniques. The results of the genetic test provide healthcare providers with actionable information to guide medication selection and dosing.
Advantages of Pharmacogenomic Testing
Pharmacogenomic testing offers several advantages in personalized medicine:
- Improved medication selection: By understanding an individual’s genetic profile, healthcare providers can select medications that are more likely to be effective based on the individual’s unique drug metabolism.
- Customized dosing: Pharmacogenomic testing can determine the optimal dosage of a medication for an individual, taking into account their genetic makeup and potential variations in drug metabolism.
- Reduced adverse reactions: By avoiding medications that may be poorly metabolized by an individual’s body, pharmacogenomic testing can help minimize the risk of adverse reactions and improve treatment outcomes.
- Guidance for alternative therapies: In cases where certain drugs may not be well-tolerated or effective based on an individual’s genetic profile, pharmacogenomic testing can provide guidance on alternative therapies that are more appropriate.
Overall, pharmacogenomic testing plays a vital role in personalized medicine by providing valuable insights into an individual’s drug metabolism and response to medication. By incorporating genetic testing into clinical practice, healthcare providers can improve treatment outcomes, enhance patient safety, and optimize medication management.
| Advantages of Pharmacogenomic Testing | Explanation |
|---|---|
| Improved medication selection | Allergy or intolerance to certain medications can be predicted based on an individual’s genetic profile, allowing for the selection of alternative drugs that will be more effective. |
| Customized dosing | Genetic variations can impact the way drugs are metabolized, influencing optimal dosages for individuals. |
| Reduced adverse reactions | By avoiding medications that may be poorly metabolized, the risk of adverse reactions is minimized. |
| Guidance for alternative therapies | Pharmacogenomics can suggest alternative therapeutic options that are better suited to an individual’s genetic makeup, improving treatment outcomes. |
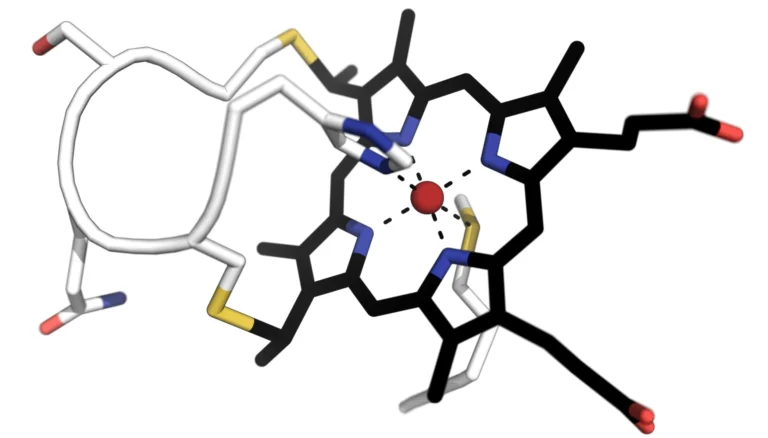
The Role of Cytochrome P450 Enzymes
Cytochrome P450 enzymes play a crucial role in drug metabolism within the body. These enzymes are responsible for metabolizing a wide range of drugs, determining how quickly or slowly they are broken down. This process has a direct impact on the efficacy and safety of medications.
Genetic variations in the genes that code for cytochrome P450 enzymes, such as CYP2B6, CYP2C19, CYP2C8, CYP2C9, CYP2D6, CYP3A4, and CYP3A5, can lead to altered drug metabolism patterns. Understanding an individual’s specific cytochrome P450 genotype allows healthcare providers to make more informed decisions regarding medication selection and dosing.
By analyzing an individual’s cytochrome P450 genotype, pharmacogenomic testing can provide valuable insights into personalized drug therapy. This information helps optimize therapeutic outcomes by tailoring medication choices to each individual’s unique genetic makeup. Pharmacogenomic testing, including cytochrome P450 genotyping, is a crucial tool in personalized medicine.
“Genetic variations in cytochrome P450 enzymes can significantly impact how medications are metabolized, leading to variations in drug response and tolerance.” – [Expert Name], [Job Title]
The Importance of Cytochrome P450 Enzymes in Drug Metabolism
Drug metabolism involves various processes that occur in the body to break down medications and eliminate them. Cytochrome P450 enzymes, located primarily in the liver but also in other tissues, play a vital role in this process. They oxidize drugs, allowing them to be eliminated from the body effectively.
Given the significant role of cytochrome P450 enzymes in drug metabolism, understanding an individual’s genetic variations in these enzymes is crucial. It can shed light on how their body will process specific medications, providing insights into potential drug interactions, therapeutic responses, and adverse reactions.
Cytochrome P450 Enzymes and Their Genetic Variations
| Cytochrome P450 Enzyme | Genes | Function |
|---|---|---|
| CYP2B6 | CYP2B6 | Metabolizes drugs such as bupropion, efavirenz, and cyclophosphamide |
| CYP2C19 | CYP2C19 | Metabolizes drugs such as omeprazole, clopidogrel, and diazepam |
| CYP2C8 | CYP2C8 | Metabolizes drugs such as paclitaxel and repaglinide |
| CYP2C9 | CYP2C9 | Metabolizes drugs such as warfarin, phenytoin, and ibuprofen |
| CYP2D6 | CYP2D6 | Metabolizes drugs such as codeine, tamoxifen, and antidepressants |
| CYP3A4 | CYP3A4 | Metabolizes drugs such as simvastatin, atorvastatin, and midazolam |
| CYP3A5 | CYP3A5 | Metabolizes drugs such as tacrolimus and nifedipine |
The genetic variations in the cytochrome P450 enzymes listed above can result in altered drug metabolism rates. Some individuals may metabolize certain medications more rapidly, leading to reduced effectiveness, while others may metabolize them more slowly, potentially resulting in toxicity.
Pharmacogenomics testing, specifically cytochrome P450 genotyping panel, provides valuable insights into an individual’s drug metabolism patterns. This knowledge enables healthcare providers to make informed decisions regarding medication selection, dosage adjustments, and personalized treatment plans that optimize therapeutic outcomes.
Benefits of Cytochrome P450 Genotyping Panel
The cytochrome P450 genotyping panel offers several advantages for personalized medication management. By identifying genetic variations in the cytochrome P450 genes, healthcare providers can determine an individual’s risk of abnormal drug metabolism. This information can guide drug selection and dosing to maximize efficacy and minimize the risk of adverse reactions.
One of the key benefits of the cytochrome P450 genotyping panel is its ability to identify individuals who are poor or rapid metabolizers of certain drugs. This knowledge allows healthcare providers to develop personalized treatment plans that take into account individual drug metabolism patterns. By considering a patient’s genetic makeup, healthcare providers can optimize medication regimens to ensure the most effective and safe treatment outcomes.
Furthermore, the personalized insights provided by the cytochrome P450 genotyping panel can help healthcare providers avoid trial and error approaches to medication management. Instead of relying solely on patient feedback or trial periods, genetic testing for drug response allows for more targeted and informed decisions. This reduces the risk of adverse reactions and improves patients’ overall experience with medication.
In addition, the cytochrome P450 genotyping panel can guide healthcare providers in selecting alternative medications or adjusting dosages for individuals who may not respond optimally to standard treatment options. By understanding an individual’s genetic profile, healthcare providers can make more precise and tailored decisions to ensure personalized and effective medication management.
“The cytochrome P450 genotyping panel provides valuable information about an individual’s drug metabolism capabilities, enabling us to make evidence-based decisions for personalized medication management.”
It is important to note that the benefits of the cytochrome P450 genotyping panel extend beyond individual patient care. This genetic testing approach also has implications for population health. By identifying genetic variations that may impact drug metabolism across different populations, healthcare providers can gain insights into how specific medications may need to be adjusted or modified for certain groups.
Overall, the cytochrome P450 genotyping panel offers healthcare providers a powerful tool for personalized medication management. By incorporating genetic testing for drug response into clinical practice, healthcare providers can optimize treatment outcomes, minimize adverse reactions, and provide more individualized care.
Specimen Collection and Testing Process
Specimen collection is an essential step in the cytochrome P450 genotyping panel process. To analyze an individual’s genetic variations associated with cytochrome P450 enzymes, a blood sample is typically collected using one of the following tubes:
- Lavender (K2EDTA)
- Pink (K2EDTA)
- Yellow (ACD solution A or B)
Once the sample is collected, it undergoes a sophisticated testing process that combines the Polymerase Chain Reaction (PCR) method with fluorescence monitoring and sequencing techniques. This testing process analyzes specific genes associated with cytochrome P450 enzymes to determine an individual’s genotype.
The cytochrome P450 genotyping panel results, providing valuable genetic information, are typically available within 5-10 days.
| Specimen Collection Tubes | Testing Process | Turnaround Time |
|---|---|---|
| Lavender (K2EDTA) | PCR, fluorescence monitoring, and sequencing | 5-10 days |
| Pink (K2EDTA) | PCR, fluorescence monitoring, and sequencing | 5-10 days |
| Yellow (ACD solution A or B) | PCR, fluorescence monitoring, and sequencing | 5-10 days |
Interpreting the Results
The results of the cytochrome p450 genotyping panel provide interpretive data on an individual’s genotype for the genes associated with cytochrome P450 enzymes. These results can be used to guide drug selection and dosing decisions.
The interpretive data may include information on drug metabolism patterns, recommendations for specific medications, and potential risks or benefits based on the genotype. Healthcare providers should refer to the detailed report provided with the test results for specific information related to each individual’s genotype.
Interpreting the results of the cytochrome p450 genotyping panel is crucial in understanding an individual’s genetic predisposition for drug metabolism. It allows healthcare providers to make informed decisions regarding drug selection and dosage, optimizing medication management for improved patient outcomes.
Limitations of Cytochrome P450 Genotyping Panel
While the cytochrome P450 genotyping panel offers valuable insights into drug metabolism patterns, it does have certain limitations. It’s important to be aware of these limitations and use the results in conjunction with other clinical factors for optimal medication management decisions.
The main limitations of the cytochrome P450 genotyping panel are as follows:
- Focus on specific cytochrome P450 genes: The panel analyzes a select group of cytochrome P450 genes involved in drug metabolism. While these genes are clinically relevant, they may not provide a comprehensive assessment of all the genes that influence drug metabolism. Other genes not included in the panel may also play a significant role in drug response and metabolism.
- Limited scope of assessment: The cytochrome P450 genotyping panel only assesses an individual’s genetic predisposition for drug response and does not consider other factors that can influence drug metabolism. Environmental factors, drug-drug interactions, and lifestyle choices can impact drug response and may not be reflected in the panel’s results.
“While the cytochrome P450 genotyping panel provides valuable genetic information, it’s important to remember that it’s just one piece of the puzzle in personalized medicine testing.”
Therefore, it is essential to interpret the results of the cytochrome P450 genotyping panel in the context of the patient’s overall clinical profile. This includes considering other clinical factors, such as medical history, current medications, and the presence of comorbidities. Taking a holistic approach to medication management ensures that the panel’s results are used in conjunction with other relevant information to make informed treatment decisions.
Example Table:
| Limitations | Explanations |
|---|---|
| Focus on specific genes | The panel only analyzes a subset of cytochrome P450 genes, potentially excluding relevant genes impacting drug metabolism. |
| Limited assessment scope | Other factors, such as drug-drug interactions and environmental influences, are not accounted for in the panel’s results. |
| Potential false negatives | The panel’s results may not always detect rare gene variants that can impact drug metabolism. |
Despite these limitations, the cytochrome P450 genotyping panel remains valuable in providing insights into drug metabolism patterns. Healthcare providers should integrate the panel’s results into a comprehensive approach to personalized medicine testing, considering all relevant clinical factors to optimize medication management and improve patient outcomes.
Clinical Applications of Cytochrome P450 Genotyping Panel
The cytochrome P450 genotyping panel offers a wide range of clinical applications, making it a valuable tool in personalized medicine testing. By analyzing an individual’s genetic variations in the cytochrome P450 genes, healthcare providers can tailor medication regimens to meet specific genetic profiles. This targeted approach can significantly improve treatment outcomes and reduce the risk of adverse reactions.
One of the key clinical applications of the cytochrome P450 genotyping panel is aiding in drug selection and dosing for medications metabolized by the cytochrome P450 enzymes. These medications include antidepressants, antipsychotics, and cancer medications.
“The cytochrome P450 genotyping panel has revolutionized the way we approach medication management. By incorporating genetic testing into our decision-making process, we can now provide personalized treatments that are safer and more effective.”
– Dr. Jane Wilson, Clinical Geneticist
Furthermore, the cytochrome P450 genotyping panel has been instrumental in improving medication management for patients with complex medical conditions. By understanding an individual’s genetic profile, healthcare providers can adjust drug dosages and identify potential drug-drug interactions, enhancing patient safety and treatment effectiveness.
Clinical Applications of Cytochrome P450 Genotyping Panel
| Medication Class | Clinical Application |
|---|---|
| Antidepressants | Optimizing drug selection and dosing based on genetic variations in cytochrome P450 enzymes |
| Antipsychotics | Personalizing medication regimens to minimize side effects and improve treatment outcomes |
| Cancer Medications | Identifying individuals at higher risk of adverse reactions and tailoring therapy accordingly |
The clinical applications of the cytochrome P450 genotyping panel extend beyond these examples, as new research continues to uncover the role of genetic variations in drug response. By harnessing the power of pharmacogenomics testing, healthcare providers can optimize medication management and provide truly individualized care.
Cytochrome P450 Genotyping Panel and Personalized Medicine
The cytochrome P450 genotyping panel is an essential tool in the field of personalized medicine. By analyzing an individual’s genetic variations in the cytochrome P450 genes, healthcare providers can tailor medication management strategies to each patient’s unique genetic profile. This approach allows for more precise drug selection and dosing, optimizing treatment outcomes and minimizing the risk of adverse reactions.
Pharmacogenetic testing, like the cytochrome P450 genotyping panel, plays a crucial role in personalized medicine. It enables healthcare providers to make evidence-based decisions by taking into account genetic information that influences drug metabolism. By understanding how an individual’s genotype affects drug response, healthcare professionals can make informed choices to improve patient care and treatment efficacy.
With the help of the cytochrome P450 genotyping panel, healthcare providers can identify genetic variations that impact drug metabolism and response. By incorporating this information into clinical practice, personalized medicine becomes a reality, creating a more individualized approach to patient care. Pharmacogenetic testing enables healthcare providers to optimize medication management strategies, ensure safer drug regimens, and enhance treatment outcomes.
The Benefits of Personalized Medicine
Personalized medicine, made possible by the cytochrome P450 genotyping panel and other pharmacogenetic testing methods, offers several key benefits:
- Optimized Drug Selection: By understanding an individual’s genetic variations in cytochrome P450 genes, healthcare providers can choose medications that are more likely to be effective and have minimal side effects.
- Precise Dosing: Each individual’s genetic profile determines how they metabolize drugs. With personalized medicine, healthcare providers can tailor the dosage to optimize therapeutic outcomes.
- Reduced Adverse Reactions: By considering an individual’s genetic variations, healthcare providers can minimize the risk of adverse reactions and improve patient safety.
- Improved Treatment Outcomes: Personalized medicine allows for the design of treatment strategies that are better suited to individual patients, leading to improved efficacy and better overall outcomes.
By embracing personalized medicine and leveraging the insights provided by the cytochrome P450 genotyping panel, healthcare providers can revolutionize the way medications are prescribed and managed. This approach holds the promise of more effective treatments, fewer adverse reactions, and enhanced patient satisfaction.
Relevant Image
Conclusion
The cytochrome P450 genotyping panel is a revolutionary genetic testing approach that provides valuable insights into an individual’s drug metabolism patterns. By analyzing genetic variations in the cytochrome P450 genes, healthcare providers can personalize medication management strategies and optimize treatment outcomes. This personalized pharmacogenomics testing is transforming the field of medication prescription and management, allowing for more effective and safer medication regimens.
By leveraging the power of genetic information obtained through the cytochrome P450 genotyping panel, healthcare providers can make informed decisions about drug selection and dosing. This genetic testing approach enables them to tailor medication regimens to each individual’s unique genetic profile, enhancing treatment efficacy and reducing the risk of side effects.
Genetic testing for drug metabolism, such as the cytochrome P450 genotyping panel, plays a critical role in the field of personalized medicine. It enables healthcare providers to incorporate pharmacogenomic insights into clinical practice, optimizing treatment outcomes and providing more individualized care. Understanding an individual’s genetic variations related to drug metabolism can help healthcare providers select the most appropriate medications and doses, leading to improved patient outcomes and enhanced medication safety.
Frequently Asked Questions
What is a cytochrome P450 genotyping panel?
A cytochrome P450 genotyping panel is a genetic test that assesses an individual’s genetic risk of abnormal drug metabolism by analyzing specific genes involved in drug metabolism.
What is pharmacogenomics?
Pharmacogenomics, also known as pharmacogenetics, is the study of how genes affect an individual’s response to medication, analyzing genetic variations to determine how drugs are metabolized by the body.
What role do cytochrome P450 enzymes play in drug metabolism?
Cytochrome P450 enzymes are responsible for metabolizing a wide range of drugs in the body, determining how quickly or slowly a drug is metabolized, which can impact its efficacy and safety.
What are the benefits of a cytochrome P450 genotyping panel?
The panel provides personalized insights into an individual’s genetic risk of abnormal drug metabolism, aiding in drug selection and dose planning for optimized medication management and improved patient outcomes.
How is a specimen collected for the cytochrome P450 genotyping panel?
A blood sample is typically collected in a lavender (K2EDTA), pink (K2EDTA), or yellow (ACD solution A or B) tube for the testing process, which analyzes specific genes associated with cytochrome P450 enzymes.
How are the results of the cytochrome P450 genotyping panel interpreted?
The results provide interpretive data on an individual’s genotype for the genes associated with cytochrome P450 enzymes, guiding drug selection and dosing decisions for personalized medication management.
What are the limitations of the cytochrome P450 genotyping panel?
The panel focuses on specific cytochrome P450 genes and may not provide a comprehensive assessment of all genes involved in drug metabolism. It also does not consider other factors such as drug-drug interactions or environmental influences.
What are the clinical applications of the cytochrome P450 genotyping panel?
The panel aids in drug selection and dosing for medications metabolized by cytochrome P450 enzymes, such as antidepressants, antipsychotics, and cancer medications, enabling personalized medicine testing.
How does the cytochrome P450 genotyping panel contribute to personalized medicine?
By analyzing an individual’s genetic variations in the cytochrome P450 genes, healthcare providers can personalize medication management based on an individual’s genotype, optimizing treatment outcomes.
How does the cytochrome P450 genotyping panel revolutionize medication management?
By leveraging genetic information, the panel ensures more effective and safer medication regimens, tailoring drug selection and dosing to an individual’s specific genetic profile.