The Challenges and Future of Cancer Pharmacogenetics
In the words of renowned scientist Francis Collins, “Genomics promises to revolutionize the field of medicine by unlocking the mysteries of our genetic makeup.” This powerful quote sets the tone for exploring the challenges and future of cancer pharmacogenetics, a field that holds immense potential in shaping the future of oncology treatment.
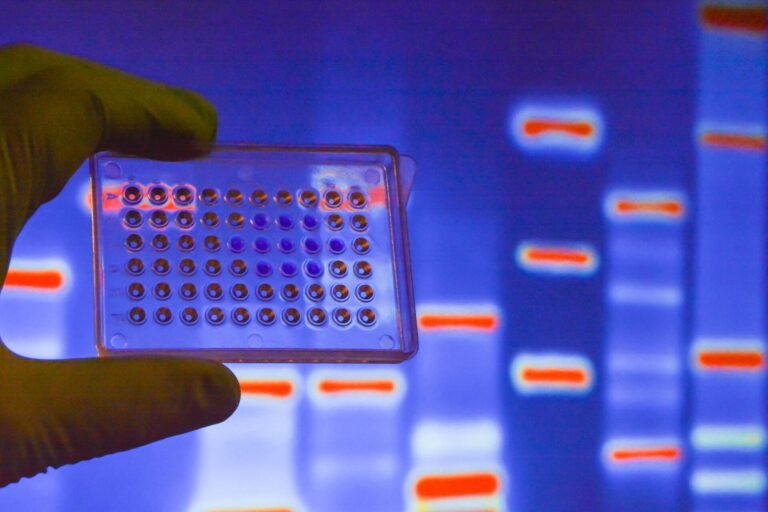
Cancer pharmacogenetics and personalized medicine are at the forefront of precision oncology, offering a new paradigm in cancer care. Through advances in genomic science and proteomics, clinicians can now develop companion diagnostics and targeted therapies that offer more precise treatment options tailored to an individual’s genetic profile.
However, as we journey into this new era of medicine, we encounter several challenges that need to be addressed. Interindividual variability in drug exposure and the potential for under or overexposure to drugs are critical factors affecting the efficacy and safety of cancer treatments. This is where pharmacogenomics research plays a crucial role, aiming to better understand drug metabolism in patients and optimize treatment options and dosages.
Despite these challenges, the field of cancer pharmacogenetics holds great promise for improving patient outcomes in precision oncology. By unlocking the power of personalized medicine, we can revolutionize cancer treatment and make significant strides towards enhancing the effectiveness and safety of therapies for individuals.
Key Takeaways:
- Cancer pharmacogenetics and personalized medicine are transforming the field of oncology by offering more precise treatment options tailored to an individual’s genetic profile.
- Interindividual variability in drug exposure and the potential for under or overexposure to drugs pose challenges in optimizing treatment efficacy and safety.
- Pharmacogenomics research aims to better understand drug metabolism in patients and optimize treatment options and dosages.
- The future of cancer pharmacogenetics holds great promise for improving patient outcomes in precision oncology.
- By unlocking the power of personalized medicine, we can revolutionize cancer treatment and enhance the effectiveness and safety of therapies for individuals.

Importance of Drug Exposure-Response Relationship in Cancer Treatment
Understanding the relationship between drug exposure and treatment response is crucial in cancer treatment. Personalized dosing based on drug exposure can help optimize treatment outcomes. Pharmacokinetic-guided dosing, which targets prespecified therapeutic concentrations or AUCs, has been successfully implemented for certain drugs like busulfan in hematopoietic cell transplantation. However, pharmacogenomics can also influence drug exposure, metabolism, and clearance. Combining pharmacogenetic testing with therapeutic drug monitoring can help individualize drug selection and dosing, leading to improved treatment outcomes.
By tailoring drug dosages to a patient’s specific pharmacokinetics, healthcare professionals can maximize the efficacy of cancer treatments while minimizing the risk of adverse events. Pharmacokinetic-guided dosing strategies take into account factors such as drug metabolism, clearance, and interpatient variability in drug exposure-response relationships.
“Understanding the drug exposure-response relationship is key to achieving optimal treatment outcomes in cancer patients.”
When it comes to cancer treatment, there is no one-size-fits-all approach. Patients respond differently to medications, and their individual characteristics influence drug disposition and response. Pharmacogenetic testing helps identify genetic variations that influence drug metabolism and response, enabling healthcare providers to tailor treatment plans to each patient’s unique genetic profile.
The utilization of pharmacogenetic testing in cancer treatment allows for the individualization of drug selection and dosing, leading to improved treatment outcomes.
For example, certain genetic variations can affect the activity of drug-metabolizing enzymes, such as cytochrome P450 enzymes, which play a crucial role in drug metabolism. These variations can impact the clearance and bioavailability of medications, potentially leading to suboptimal drug exposure or increased toxicity.
| Factors influencing drug exposure-response relationships | Impact on treatment outcomes |
|---|---|
| Genetic variations in drug-metabolizing enzymes | Altered drug metabolism, clearance, and bioavailability |
| Pharmacokinetic variability | Inconsistent drug exposure among patients |
| Interpatient variability in drug response | Differences in treatment efficacy and toxicity |
By incorporating pharmacogenetic testing into cancer treatment plans, healthcare professionals can gain valuable insights into how individual patients are likely to respond to specific medications. This information can guide the selection of appropriate medications and optimize dosing regimens to achieve the desired therapeutic effect.
Supportive Care in Cancer and the Role of Pharmacogenetics
Supportive care in cancer plays a crucial role in managing and preventing treatment-related side effects, aiming to improve the quality of life for patients. However, there are pharmacogenetic variations that can lead to drug exposure variability, increasing the risk of side effects and suboptimal treatment outcomes.
Pharmacogenetic testing can help identify patients who may be at risk due to these variations and guide alternative drug choices or dosage adjustments for optimal supportive care. By understanding a patient’s genetic makeup, healthcare providers can personalize the treatment plan and mitigate the risks associated with drug exposure variability.
One example of how pharmacogenetics can impact supportive care is the metabolism of ondansetron, an antiemetic used to manage nausea and vomiting in cancer patients. Ultrarapid metabolizers of ondansetron may experience underexposure to the drug, leading to breakthrough symptoms. Similarly, patients who are poor metabolizers of CYP2C19 may be at risk for underexposure to voriconazole, an antifungal medication, increasing their susceptibility to fungal infections.
By selectively testing for pharmacogenetic variations, healthcare providers can ensure appropriate drug selection and dosing to optimize supportive care outcomes and reduce the risk of adverse events. Incorporating pharmacogenetic testing into routine supportive care protocols empowers healthcare professionals to deliver personalized treatment strategies for each patient based on their unique genetic profile.
| Impact of Pharmacogenetic Variations on Supportive Care | Pharmacogenetic Variation | Drug | Risk |
|---|---|---|---|
| Ultrarapid Metabolism | Ondansetron metabolism | Ondansetron | Underexposure, breakthrough symptoms |
| CYP2C19 Poor Metabolism | Voriconazole metabolism | Voriconazole | Underexposure, increased risk of fungal infections |
The integration of pharmacogenetics into supportive care practices represents a significant advancement in delivering personalized medicine to cancer patients. By leveraging genetic information, healthcare providers can optimize drug selection, dosage, and administration, leading to improved outcomes and enhanced patient well-being.
Through pharmacogenetic testing, healthcare providers can identify patients at risk for drug exposure variability and tailor supportive care to suit individual needs. This integration of genetics and medicine empowers healthcare professionals to deliver high-quality care that is both effective and personalized.
Pharmacogenetics of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used for pain management in cancer patients. However, the effectiveness and safety of NSAIDs can vary based on the individual’s genetic makeup. One important genetic factor that affects the metabolism of NSAIDs is the CYP2C9 genotype, which is responsible for the enzyme that metabolizes these drugs.
The CYP2C9 gene has several allelic variants, including CYP2C9*2 and CYP2C9*3, that result in reduced enzyme activity. Individuals who carry these variants may experience altered drug metabolism and increased drug exposure when taking NSAIDs. This can lead to a higher risk of drug toxicity and adverse effects.
Pharmacogenetic testing can help identify patients with specific CYP2C9 genotypes, allowing healthcare providers to adjust the dosage or choose alternative pain management strategies for optimal treatment outcomes. By incorporating genetic information into the decision-making process, healthcare professionals can personalize the treatment plan and minimize the risks associated with NSAID therapy.
A comprehensive table outlining the different CYP2C9 genotypes and their impact on NSAID metabolism and efficacy can be seen below:
| CYP2C9 Genotype | Enzyme Activity | NSAID Metabolism | Effect on Drug Exposure |
|---|---|---|---|
| Normal Metabolizer (CYP2C9*1/*1) | Normal | Efficient | Standard |
| Intermediate Metabolizer (CYP2C9*1/*2 or CYP2C9*1/*3) | Reduced | Altered | Increased |
| Poor Metabolizer (CYP2C9*2/*2, CYP2C9*2/*3, or CYP2C9*3/*3) | Virtually Absent | Markedly Altered | Significantly Increased |
It is important for healthcare providers to consider the CYP2C9 genotype when prescribing NSAIDs to cancer patients. By tailoring the treatment plan based on an individual’s pharmacogenetic profile, healthcare professionals can improve pain management outcomes and reduce the risk of adverse drug effects.
Opioid Pharmacogenetics and Individualized Pain Management
Opioids are commonly used for managing severe pain in cancer patients. The metabolism of opioids, such as codeine and tramadol, is influenced by CYP2D6 activity. Poor metabolizers may not effectively convert these prodrugs into their active forms, resulting in reduced pain relief. Pharmacogenetic testing can help identify patients with altered CYP2D6 metabolism and inform individualized pain management strategies, such as choosing alternative opioids or adjusting dosages for optimal pain control.
| Opioid | Metabolism influenced by CYP2D6 | Management strategies |
|---|---|---|
| Codeine | Converted to morphine by CYP2D6 |
|
| Tramadol | Metabolized to active metabolite by CYP2D6 |
|
Individualized pain management for cancer patients involves tailoring opioid selection and dosing based on an individual’s genetic profile. By understanding the impact of CYP2D6 metabolism on opioid efficacy, healthcare providers can optimize pain control and minimize the risk of adverse effects.
Role of Pharmacogenetics in Cancer-Related Nausea and Vomiting
Nausea and vomiting are common side effects of cancer treatment. Patients undergoing chemotherapy or radiation therapy often experience these symptoms, which can significantly impact their quality of life. To manage these side effects, antiemetic medications are commonly prescribed. However, the effectiveness of antiemetics can vary among individuals due to genetic factors, specifically the CYP2D6 metabolism enzyme.
CYP2D6 is responsible for metabolizing many antiemetics, including ondansetron, a commonly used medication for nausea and vomiting in cancer patients. The activity of CYP2D6 can vary among individuals, leading to differences in drug metabolism and drug-exposure relationships. Ultrarapid metabolizers, who have increased CYP2D6 activity, may experience suboptimal drug exposure, leading to breakthrough symptoms despite medication use. On the other hand, poor metabolizers may have reduced drug metabolism, resulting in higher drug concentrations and an increased risk of side effects.
Pharmacogenetic testing can play a crucial role in identifying patients at risk for altered drug metabolism and help guide personalized antiemetic choices or dosage adjustments. By understanding an individual’s CYP2D6 metabolism status, healthcare providers can tailor antiemetic therapy to optimize drug-exposure relationships and improve symptom control.
Table: The Impact of CYP2D6 Metabolism on Antiemetic Efficacy
| CYP2D6 Metabolizer Status | Impact on Antiemetic Efficacy |
|---|---|
| Ultrarapid Metabolizer | Underexposure to antiemetic, breakthrough symptoms |
| Extensive Metabolizer | Optimal drug exposure, effective symptom control |
| Intermediate Metabolizer | Possible variations in drug exposure and symptom control |
| Poor Metabolizer | Possible overexposure to antiemetic, increased risk of side effects |
Identifying patients with altered CYP2D6 metabolism through pharmacogenetic testing can inform alternative antiemetic choices or dosage adjustments for optimal control of nausea and vomiting. This personalized approach to antiemetic therapy can help minimize side effects, improve treatment adherence, and enhance the overall quality of life for cancer patients undergoing treatment.
“Pharmacogenetic testing can play a crucial role in identifying patients at risk for altered drug metabolism and help guide personalized antiemetic choices or dosage adjustments.”
Pharmacogenetics of Antifungal Therapy in Cancer Patients
Cancer patients undergoing immunosuppressive therapy are at risk for fungal infections, necessitating the use of antifungal therapy. One commonly used antifungal drug is voriconazole, which is metabolized by the enzyme CYP2C19. However, the activity of CYP2C19 can vary among individuals, leading to differences in drug metabolism and subsequent drug exposure variability.
Poor metabolizers of voriconazole may experience underexposure to the drug, resulting in inadequate therapeutic effect and an increased risk of treatment failure. On the other hand, ultrarapid metabolizers may experience overexposure to voriconazole, increasing the risk of toxicity.
To optimize antifungal therapy in cancer patients, pharmacogenetic testing can be utilized. By determining a patient’s CYP2C19 metabolism status, healthcare providers can identify individuals at risk for altered drug metabolism and make informed decisions regarding alternative antifungal choices or dosage adjustments.
Here is an overview of the different CYP2C19 metabolism phenotypes:
- Extensive metabolizers (EM): These individuals have normal CYP2C19 metabolism and are not expected to have significant changes in drug exposure compared to the general population.
- Poor metabolizers (PM): Poor metabolizers have reduced or no functional CYP2C19 enzyme activity, leading to reduced drug metabolism. This can result in higher drug exposure and an increased risk of adverse effects.
- Ultrarapid metabolizers (UM): Ultrarapid metabolizers have increased CYP2C19 enzyme activity, leading to faster drug metabolism. This can result in lower drug exposure and a potential lack of therapeutic effect.
Table: CYP2C19 Phenotypes and Drug Exposure Variability in Cancer Patients
| CYP2C19 Phenotype | Drug Exposure | Clinical Implications |
|---|---|---|
| Extensive metabolizers (EM) | Normal | No significant changes in drug exposure expected |
| Poor metabolizers (PM) | Increased | Higher risk of adverse effects |
| Ultrarapid metabolizers (UM) | Decreased | Potential lack of therapeutic effect |
Pharmacogenetic testing, combined with clinical monitoring, can help optimize antifungal therapy by individualizing treatment choices and doses based on a patient’s CYP2C19 metabolism status. This approach minimizes the risk of treatment failure and reduces the likelihood of adverse effects associated with antifungal therapy.
Pharmacogenetic testing allows healthcare providers to tailor antifungal therapy in cancer patients based on individual CYP2C19 metabolism, optimizing treatment outcomes and minimizing the risk of adverse effects.

Challenges and Opportunities for Implementing Pharmacogenetics in Cancer Care
Despite the potential benefits of pharmacogenetic testing in cancer care, there are several barriers to its widespread clinical implementation. These challenges include:
- Limited robust clinical trials to establish the efficacy and safety of pharmacogenetic testing in cancer treatment.
- Barriers to accessing real-time pharmacogenetic testing results at the point of care, hindering immediate clinical decision-making.
- A lack of education and awareness among healthcare providers on how to interpret and apply pharmacogenetic testing results in practice.
- Cost considerations, as implementing pharmacogenetic testing requires investment in infrastructure, technology, and training.
Despite these challenges, there are significant opportunities for overcoming these barriers and integrating pharmacogenetics into routine cancer care:
- Increasing awareness and education: Healthcare providers need to be informed about the benefits and practical application of pharmacogenetic testing to ensure effective implementation.
- Integrating testing into electronic health record systems: By incorporating pharmacogenetic testing results into EHRs, healthcare providers can access and utilize the information readily during clinical decision-making.
- Fostering collaborations: Researchers, clinicians, and policymakers should collaborate to drive the adoption and implementation of pharmacogenetics in cancer care, sharing best practices and addressing challenges collectively.
Overcoming these challenges and seizing these opportunities will pave the way for the widespread integration of pharmacogenetics into routine cancer care, ensuring personalized and optimized treatment for cancer patients.
| Barriers | Opportunities |
|---|---|
| Limited robust clinical trials | Increasing awareness and education |
| Barriers to accessing results in real-time at the point of care | Integrating testing into electronic health record systems |
| Lack of education and awareness on how to apply the results in practice | Fostering collaborations between researchers, clinicians, and policymakers |
| Cost considerations |
Resources for Evaluating Pharmacogenetic Effects on Drug Response
When it comes to evaluating the pharmacogenetic effects on drug response, there are several valuable resources available. These resources provide clinicians, researchers, and labs with critical information for assessing the clinical relevance of drug-gene interactions and incorporating pharmacogenetics into medication management processes.
- Clinical Pharmacogenetics Implementation Consortium (CPIC): The CPIC is a consortium of experts in pharmacogenomics that develops guidelines to translate pharmacogenetic test results into actionable prescribing decisions. These guidelines are designed to help healthcare providers navigate the complex relationship between genetic variations and drug response, ensuring safe and effective medication management.
- Pharmacogenomics Knowledgebase (PharmGKB): The PharmGKB is a comprehensive knowledgebase that curates information about the impact of genetic variation on drug response. It provides clinicians and researchers with access to a wealth of data on drug-gene interactions, including dosing recommendations, specific gene-drug associations, and clinical annotations for various medications.
- Pharmacogene Variation (PharmVar) Consortium: The PharmVar Consortium focuses on allelic variation in pharmacogenes, which are genes that influence drug response and metabolism. By cataloging these genetic variations, the PharmVar Consortium aims to provide researchers and clinicians with a better understanding of how genetic differences can affect drug efficacy and safety.
These resources serve as invaluable references for assessing the impact of pharmacogenetics on drug response. By leveraging the guidelines and curated knowledge from the CPIC, PharmGKB, and PharmVar Consortium, healthcare professionals can make informed decisions that optimize medication management and improve patient outcomes.
The Role of Pharmacogenetics in Personalized Cancer Treatment
Pharmacogenetics plays a crucial role in the field of personalized cancer treatment, leveraging advancements in genomic medicine to customize therapeutic approaches for individual patients. By identifying genetic variations that influence drug metabolism and response, pharmacogenetics enables oncologists to make more informed treatment decisions and optimize therapy outcomes. Through pharmacogenetic testing, healthcare providers can identify patients who are likely to respond positively to specific targeted therapies, while avoiding unnecessary side effects or treatment failure.
Genomic medicine has revolutionized cancer treatment by allowing clinicians to tailor therapies based on the specific genetic makeup of each patient. By deciphering the genetic information encoded in an individual’s DNA, oncologists can identify molecular alterations driving the growth of cancerous cells. This knowledge guides the selection of targeted therapies that directly interfere with the mechanisms responsible for tumor proliferation.
The integration of pharmacogenetics into personalized cancer treatment holds great promise for improving patient outcomes by optimizing therapy effectiveness. It allows healthcare providers to design treatment plans that are precisely aligned with each patient’s genetic profile and the specific characteristics of their cancer. By tailoring therapies based on individual genetic variations, oncologists can maximize the efficacy of treatment while minimizing unnecessary drug exposure and potential side effects.
An example of the application of pharmacogenetics in personalized cancer treatment is the use of genetic testing to identify patients who will respond favorably to specific targeted therapies. For instance, in certain types of breast cancer, the HER2 gene amplification is associated with a more aggressive form of the disease. However, drugs such as trastuzumab specifically target cells with HER2 amplification, effectively inhibiting tumor growth. Pharmacogenetic testing can identify patients who are HER2-positive and likely to respond to trastuzumab, enabling oncologists to tailor treatment plans and improve patient outcomes.
Pharmacogenetics also plays a vital role in predicting and managing potential side effects of cancer therapies. By analyzing genetic variations that affect drug metabolism or drug targets, healthcare providers can anticipate adverse reactions and adjust treatment accordingly. For example, some patients may have genetic variations that affect the metabolism of chemotherapy drugs, leading to increased toxicity or treatment failure. Pharmacogenetic testing can help identify such variations and guide oncologists in selecting alternative treatment options or adjusting drug dosages to achieve optimal therapeutic outcomes.
The Benefits of Pharmacogenetics in Personalized Cancer Treatment
The integration of pharmacogenetics into personalized cancer treatment offers several key benefits:
- Improved treatment outcomes: By tailoring therapies based on individual genetic variations, pharmacogenetics enhances treatment effectiveness and reduces the risk of adverse reactions.
- Enhanced patient safety: Identifying genetic variations that influence drug metabolism and response allows healthcare providers to avoid medications that may cause severe side effects in certain individuals.
- Optimized therapy selection: Pharmacogenetic testing helps identify patients who are likely to respond to specific targeted therapies, allowing for the selection of the most appropriate treatment regimen.
- Reduced healthcare costs: By optimizing treatment plans and avoiding unnecessary drug exposure, pharmacogenetics has the potential to reduce healthcare costs associated with ineffective or poorly tolerated therapies.
Overall, the integration of pharmacogenetics into personalized cancer treatment represents a significant advancement in precision medicine. By tailoring therapies based on individual genetic variations, healthcare providers can offer more effective and safer treatment options to cancer patients. As genomic medicine continues to advance, the role of pharmacogenetics in personalized cancer treatment is expected to become even more prominent, optimizing therapy outcomes and improving patient care.
Sources:
Miller NA, et al. Pharmacogenomics. Precision medicine in the oncology clinic. Nat Biotechnol. 2012;30(7):621–623.
McLeod HL. Pharmacogenetics: heralding a new era in personalized healthcare? Hum Genomics. 2010;4(4):239–244.
Future Directions in Cancer Pharmacogenetics
The field of cancer pharmacogenetics is continuously evolving, with a focus on advancing personalized cancer treatment and optimizing patient outcomes. Several future directions have been identified, including:
- Expanding Clinical Trials: Increasing the number and scope of clinical trials will generate more robust evidence for drug-gene interactions and enable the development of targeted therapies based on genetic profiles. This will enhance treatment efficacy and minimize adverse effects.
- Improving Point-of-Care Testing: Enhancing access to real-time pharmacogenetic results at the point of care will enable healthcare providers to make informed treatment decisions promptly. Point-of-care testing allows for timely adjustments to medication regimens, optimizing therapy outcomes.
- Integrating Pharmacogenetics into Cancer Care Guidelines: Incorporating pharmacogenetic testing into routine cancer care guidelines will ensure standardized and systematic implementation. This integration will enable healthcare professionals to utilize genetic information effectively for selecting drugs and dosing strategies tailored to individual patients.
These future directions will drive the widespread implementation of pharmacogenetics in oncology practice, revolutionizing cancer treatment worldwide. Ongoing research, collaborations, and advancements in technology will continue to propel the field forward, improving patient outcomes through optimized pharmacotherapy.
Conclusion
Cancer pharmacogenetics presents both challenges and opportunities for improving patient care in oncology. The field holds great promise for advancing precision oncology and optimizing drug selection and dosing for individual patients. However, there are barriers to the widespread implementation of pharmacogenetics, including limited clinical trials and a lack of education in how to apply the results in practice.
Despite these challenges, there are significant opportunities for harnessing the potential of pharmacogenetics. By addressing the barriers and leveraging available resources and technologies, pharmacogenetic testing can be integrated into routine cancer care. This integration can lead to more personalized treatment options and improved patient outcomes.
The future of cancer pharmacogenetics is bright. As awareness grows and education becomes more widespread, the field will continue to advance. Collaborations between researchers, clinicians, and policymakers will play a crucial role in overcoming challenges and driving the implementation of pharmacogenetics in oncology. By embracing these opportunities and optimizing drug therapies, we have the potential to revolutionize cancer care and improve the lives of patients around the world.
FAQ
What is cancer pharmacogenetics?
Cancer pharmacogenetics is the study of how an individual’s genetic makeup influences their response to cancer treatment drugs. It aims to optimize treatment outcomes and minimize side effects by identifying genetic variations that impact drug metabolism and response.
How does drug exposure-response relationship affect cancer treatment?
The relationship between drug exposure and treatment response is crucial in cancer treatment. Personalized dosing based on drug exposure can help optimize treatment outcomes. Pharmacogenomic testing can identify variations in drug metabolism and clearance, guiding individualized drug selection and dosing.
What role does pharmacogenetics play in cancer supportive care?
Pharmacogenetic variations can impact drug exposure variability and increase the risk of side effects in cancer supportive care. Pharmacogenetic testing can identify patients at risk and inform alternative drug choices or adjust dosages for optimal supportive care outcomes.
How does pharmacogenetics affect the metabolism of non-steroidal anti-inflammatory drugs (NSAIDs) in cancer patients?
Variations in CYP2C9 genotype can influence the metabolism and plasma concentrations of NSAIDs in cancer patients. Pharmacogenetic testing can identify patients at risk for altered drug metabolism and inform dose adjustments for optimal pain management outcomes.
How does pharmacogenetics impact opioid pharmacotherapy in cancer patients?
The metabolism of opioids, such as codeine and tramadol, is influenced by CYP2D6 activity. Pharmacogenetic testing can identify patients with altered CYP2D6 metabolism and inform individualized pain management strategies, such as choosing alternative opioids or adjusting dosages for optimal pain control.
How does pharmacogenetics affect the metabolism of antiemetics in cancer patients?
The metabolism of antiemetics, such as ondansetron, can be influenced by CYP2D6 activity. Pharmacogenetic testing can help identify patients at risk for altered drug metabolism and inform alternative antiemetic choices or adjust dosages for optimal control of nausea and vomiting.
How does pharmacogenetics impact antifungal therapy in cancer patients?
The metabolism of antifungal drugs like voriconazole is influenced by CYP2C19 activity. Pharmacogenetic testing can help identify patients at risk for altered drug metabolism and inform alternative antifungal choices or adjust dosage for optimal treatment outcomes.
What are the challenges and opportunities for implementing pharmacogenetics in cancer care?
Challenges include limited clinical trials, barriers to accessing results at the point of care, lack of education on how to apply results in practice, and cost considerations. Opportunities include increasing awareness among healthcare providers, integrating pharmacogenetic testing into electronic health records, and fostering collaborations.





3 Comments