What is the CYP2D6 Gene and How Does it Metabolize?

The CYP2D6 gene is a critical component of drug metabolism and plays a significant role in the field of pharmacogenomics. This gene is responsible for breaking down medications like codeine and tricyclic antidepressants, converting them into active or inactive forms. With over 100 known variations, the CYP2D6 gene exhibits different levels of enzyme activity, impacting how individuals respond to medications.
Key Takeaways:
- The CYP2D6 gene is important in drug metabolism and pharmacogenomics.
- It metabolizes drugs like codeine and tricyclic antidepressants.
- The gene has over 100 known variations, leading to different levels of enzyme activity.
- CYP2D6 gene variations impact how individuals respond to medications.
- Understanding the function of CYP2D6 is vital in personalized medicine and optimizing drug therapy.
The Importance of CYP2D6 in Drug Metabolism
CYP2D6, a key enzyme involved in drug metabolism, plays a critical role in determining how individuals respond to certain medications. The genetic variations within the CYP2D6 gene can lead to different levels of enzyme activity, resulting in distinct medication responses and pharmacokinetics. These genetic variations range from poor metabolizers, who have reduced enzyme activity, to ultra-rapid metabolizers, who have increased enzyme activity.
By understanding a patient’s CYP2D6 phenotype, healthcare providers can tailor drug therapy to optimize treatment outcomes and prevent adverse drug reactions. Individualized drug dosing based on CYP2D6 activity levels can enhance medication effectiveness and minimize the risk of side effects.
CYP2D6 enzyme activity levels can be determined through genetic testing, allowing healthcare providers to classify patients into different metabolic phenotypes. This information enables clinicians to make informed decisions regarding medication selection, dosing adjustments, and the potential need for alternative therapies.
For example, individuals with reduced CYP2D6 enzyme activity may require lower doses of certain drugs to achieve therapeutic effects, while those with increased activity may need higher doses to attain the same outcome.
“CYP2D6 enzyme activity is a crucial factor in pharmacokinetics, which ultimately affects how the body processes medications. Genetic variations in the CYP2D6 gene can significantly impact medication response and determine whether a patient will experience the desired therapeutic effects or potential adverse reactions.”
Understanding the importance of CYP2D6 in drug metabolism is vital for providing personalized medicine and optimizing patient care. Through genetic testing and analysis, healthcare providers can identify and interpret CYP2D6 genetic variations, leading to more precise and tailored pharmacotherapy.
| CYP2D6 Phenotype | Enzyme Activity Level | Medication Response |
|---|---|---|
| Poor Metabolizers | Reduced or absent enzyme activity | Increased risk of adverse drug reactions |
| Intermediate Metabolizers | Partial enzyme activity | Variable medication response |
| Normal Metabolizers | Typical enzyme activity | Standard medication response |
| Ultra-Rapid Metabolizers | Increased enzyme activity | Potentially decreased medication efficacy |
This table outlines the different CYP2D6 phenotypes, their corresponding enzyme activity levels, and their influence on medication response. It highlights how gene variations can contribute to varying drug metabolism rates and, consequently, the efficacy and safety of pharmacotherapy.
Understanding the role of CYP2D6 in drug metabolism is crucial for optimizing patient care, minimizing adverse reactions, and achieving the desired therapeutic outcomes.
Role of CYP2D6 in Pharmacogenetics
In the field of pharmacogenetics, the study of CYP2D6 focuses on understanding how genetic variations in this specific gene can influence an individual’s response to medications. The CYP2D6 gene is known to play a crucial role in drug metabolism, and its genetic variations can lead to variations in drug efficacy, metabolism, and susceptibility to side effects.
By identifying a patient’s specific CYP2D6 genotype, healthcare providers can personalize drug therapy to optimize treatment outcomes and minimize the risk of adverse drug reactions. Genetic variations in CYP2D6 contribute to the variability observed in medication response among individuals.
Pharmacogenetics plays a pivotal role in the advancement of precision medicine, allowing for tailored treatment strategies based on an individual’s genetic makeup. The CYP2D6 gene is just one example of how genetic variations can influence drug therapy and personalizing medicine.
To better grasp the impact of CYP2D6 genetic variations on drug response, let’s take a closer look at the different CYP2D6 phenotypes and their implications:
1. Poor Metabolizers
Individuals classified as poor metabolizers have reduced or no enzyme activity due to specific genetic variations in the CYP2D6 gene. As a result, drugs that rely on CYP2D6 metabolism may not be effectively broken down, leading to potential treatment failure or inadequate response.
2. Intermediate Metabolizers
Intermediate metabolizers have reduced enzyme activity compared to normal metabolizers due to specific genetic variations. This phenotype can result in variable drug response, and dosage adjustments may be necessary to achieve the desired therapeutic effect.
3. Extensive Metabolizers
Extensive metabolizers have normal CYP2D6 enzyme activity and are considered the “average” metabolic phenotype. This group typically metabolizes medications in the expected manner, leading to normal drug response and efficacy.
4. Ultra-Rapid Metabolizers
Ultra-rapid metabolizers have genetic variations that result in increased CYP2D6 enzyme activity. Consequently, drugs metabolized by CYP2D6 may be rapidly broken down, leading to reduced drug efficacy or even potential toxicity. Adjustments to drug dosages may be necessary for this population.
Understanding the different CYP2D6 phenotypes can guide healthcare providers in selecting appropriate drug therapies and tailoring dosages based on an individual’s genetic makeup. This personalized approach helps optimize treatment outcomes while minimizing the risk of adverse drug reactions specific to CYP2D6 metabolism.
Pharmacogenetics, with a focus on CYP2D6, not only enhances our current understanding of how genetic variations influence medication response but also opens doors to improved precision medicine strategies. By incorporating an individual’s genetic profile, healthcare providers can optimize drug therapy, resulting in better patient outcomes and personalized care.
Table: CYP2D6 Phenotypes and Their Implications
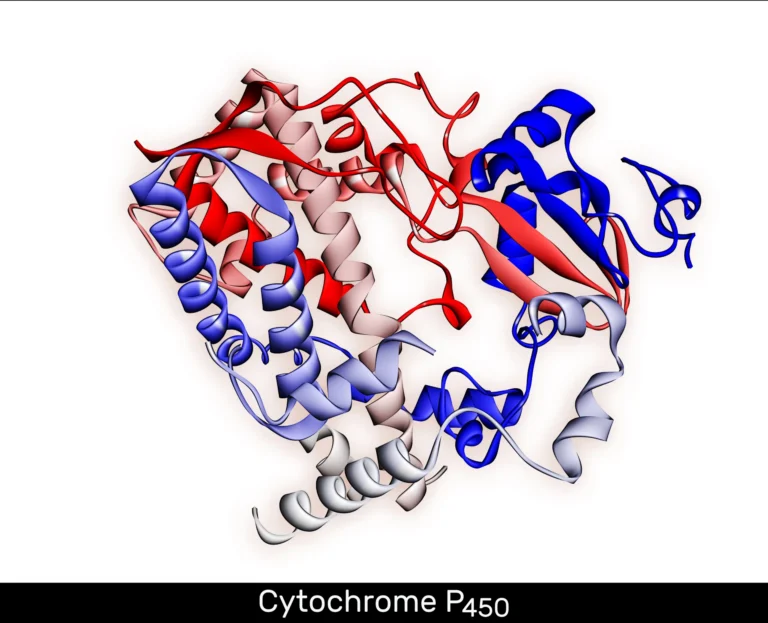
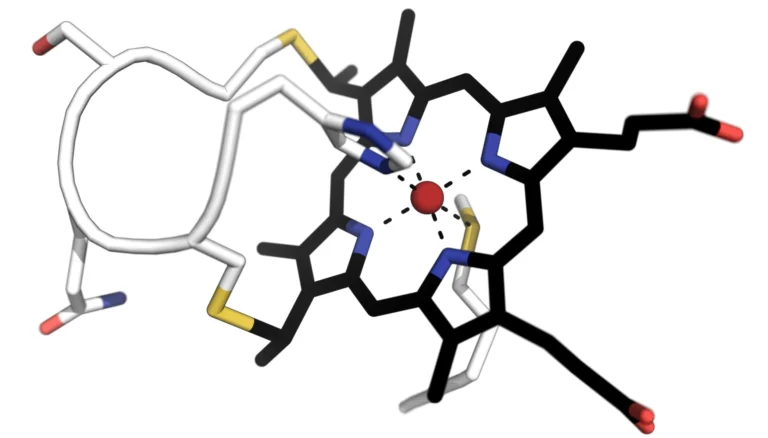
Structure and Function of CYP2D6
CYP2D6, a member of the cytochrome P450 enzyme family, is crucial for drug metabolism. This family of enzymes is responsible for metabolizing various drugs and substances, including CYP2D6’s specific role in drug breakdown. By binding to specific drugs, CYP2D6 facilitates the conversion of these substances into metabolites.
The structure of CYP2D6 enables it to interact with specific drugs, allowing effective metabolization. This interaction involves the active site of the enzyme binding to the drug molecule, initiating the breakdown process. The mechanism by which CYP2D6 operates ensures the efficient metabolism of drugs, impacting their efficacy and potential side effects.
Genetic variations can affect the function of CYP2D6 and alter drug metabolism. These variations can lead to different enzyme activity levels, ranging from normal metabolizers to poor metabolizers or ultra-rapid metabolizers. Poor metabolizers may have decreased or no enzyme activity, impacting drug efficacy and increasing the risk of adverse drug reactions. Conversely, ultra-rapid metabolizers have increased enzyme activity, potentially resulting in inadequate drug concentration for therapeutic effect.
Understanding the structure and function of CYP2D6 is vital for predicting drug response and optimizing drug therapy. Pharmacogenetic testing can help identify genetic variations in CYP2D6 that may affect enzyme function, thereby influencing treatment decisions and dosing adjustments.
Table 1: Common Substrates and Inhibitors of CYP2D6
| Substrates | Inhibitors |
|---|---|
| Codeine | Fluoxetine |
| Tramadol | Paroxetine |
| Amitriptyline | Quinidine |
Table 1 displays common substrates and inhibitors of CYP2D6. Substrates are drugs metabolized by CYP2D6, while inhibitors interfere with the enzyme’s activity, potentially affecting the metabolism of these drugs. Awareness of these interactions is crucial in the context of drug therapy optimization.
Regulation and Expression of CYP2D6
The expression and activity levels of CYP2D6 can vary between individuals due to genetic and environmental factors. Factors such as drug interactions, age, sex, and disease conditions can influence the regulation of CYP2D6 gene expression and enzyme activities. Genetic variations, including gene duplications, deletions, and single nucleotide polymorphisms, can also impact the function of CYP2D6.
Understanding the regulation and expression of CYP2D6 is crucial in interpreting and predicting drug metabolism and response. These factors play a significant role in determining an individual’s ability to metabolize specific medications. Genetic variations can affect the enzyme’s activity, potentially leading to variations in drug efficacy and the occurrence of adverse drug reactions.
Research has shown that individuals with certain genetic variations in CYP2D6 may be poor metabolizers, while others may be extensive metabolizers or ultra-rapid metabolizers. These variations can have significant implications for drug therapy, as they can impact drug dosing requirements and therapeutic outcomes.
By understanding the regulation and expression of CYP2D6, researchers and healthcare providers can better identify patients who may be at risk of altered drug metabolism. This knowledge can help guide personalized medicine approaches, allowing for tailored drug therapy based on an individual’s genetic variation in CYP2D6.
| Factors Affecting CYP2D6 Regulation | Impact on Enzyme Activities |
|---|---|
| Drug interactions | Affect drug metabolism and response |
| Age | May alter enzyme activities |
| Sex | Gender differences in CYP2D6 expression |
| Disease conditions | Can affect enzyme activities and drug metabolism |
| Genetic variations | Impact CYP2D6 function and drug metabolism |
Understanding the regulation and expression of CYP2D6 is an ongoing area of research. By further exploring the interplay between genetic and environmental factors, scientists can gain deeper insights into the complex mechanisms driving CYP2D6-mediated drug metabolism.
Clinical Implications of CYP2D6 Variability
The variability of CYP2D6 activity has significant clinical implications. Individuals with poor metabolizers, characterized by reduced or no enzyme activity, may require lower drug doses to avoid toxic effects. Conversely, ultra-rapid metabolizers, who have increased enzyme activity, may require higher doses to achieve therapeutic effects. Proper drug dosing based on an individual’s CYP2D6 phenotype is crucial to optimize treatment outcomes and minimize adverse drug reactions.
For specific medications like codeine and tricyclic antidepressants, the dosing should be adjusted considering an individual’s CYP2D6 phenotype. Poor metabolizers may be more prone to adverse drug reactions, and therefore, lower drug doses can help avoid these complications. On the other hand, ultra-rapid metabolizers may require higher doses to achieve the desired effect due to their rapid drug metabolism.
CYP2D6 variability is especially relevant in personalized medicine, where treatment plans are tailored to an individual’s genetic profile. By understanding an individual’s CYP2D6 phenotype, healthcare providers can optimize drug dosing, improve treatment efficacy, and minimize the risk of adverse drug reactions. This approach promotes a more targeted and individualized approach to patient care.
“Consideration of an individual’s CYP2D6 phenotype is essential for safe and effective drug therapy, as poor metabolizers and ultra-rapid metabolizers require different dosing strategies to achieve optimal treatment outcomes.”
To illustrate the clinical implications of CYP2D6 variability, the following table summarizes the recommended drug dosing for poor metabolizers and ultra-rapid metabolizers:
| Medication | Poor Metabolizers | Ultra-Rapid Metabolizers |
|---|---|---|
| Codeine | Lower dose to avoid toxicity | Higher dose for therapeutic effect |
| Tricyclic antidepressants | Lower dose to avoid side effects | Higher dose for therapeutic effect |
By considering CYP2D6 variability and tailoring drug dosing accordingly, healthcare providers can significantly improve patient safety and treatment outcomes. Understanding an individual’s CYP2D6 phenotype is a critical component of precision medicine, as it allows for personalized and optimized drug therapy.
Implementation of CYP2D6 Testing
Implementing CYP2D6 testing in clinical practice is a crucial step towards personalized medicine and optimizing drug therapy. Pharmacogenomics testing, which involves genotyping or phenotype testing, can provide valuable insights into an individual’s CYP2D6 activity and guide treatment decisions. By analyzing a patient’s CYP2D6 genotype or phenotype, healthcare providers can tailor drug therapy to maximize efficacy and minimize the risk of adverse drug reactions.
The ability to identify an individual’s CYP2D6 activity level allows for a more precise approach in drug therapy. It helps healthcare providers understand how a patient may metabolize specific medications, enabling them to adjust doses accordingly and select alternative drugs if needed. This personalized approach to drug therapy aims to enhance treatment outcomes and improve patient safety.
CYP2D6 testing is particularly recommended for medications known to interact with the enzyme, such as codeine, tramadol, and amitriptyline. These medications can be influenced by CYP2D6 activity, leading to variations in drug response and potential adverse effects. Guidelines from reputable organizations, such as the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetics Working Group (DPWG), provide recommendations for CYP2D6 testing and drug dosing based on genotype or phenotype.
By incorporating CYP2D6 testing into clinical practice, healthcare providers can make more informed decisions regarding drug therapy, improving patient outcomes and preventing avoidable adverse drug reactions. With the advancement of pharmacogenomics and personalized medicine, the implementation of CYP2D6 testing holds great potential in revolutionizing drug therapy and optimizing patient care.
Benefits of CYP2D6 Testing in Drug Therapy:
- Individualized drug therapy based on CYP2D6 activity levels
- Optimization of drug dosing for better treatment outcomes
- Reduced risk of adverse drug reactions and side effects
- Identification of alternative medications for individuals with atypical CYP2D6 activity
- Enhanced patient safety and improved medication management
By embracing the implementation of CYP2D6 testing, healthcare providers can harness the power of pharmacogenomics to deliver personalized medicine and optimize drug therapy for each individual patient.

Image: CYP2D6 testing is key to personalized medicine and optimized drug therapy.
Challenges and Future Directions in CYP2D6 Research
Despite significant progress in understanding the role of CYP2D6 in drug metabolism, there are still challenges in accurately predicting drug response based on genotype or phenotype. The complexity and diversity of genetic variations in CYP2D6 pose difficulties in determining enzyme activity and drug metabolism with precision. As a result, further research is essential to enhance our understanding of CYP2D6 functionality and its impact on drug therapy.
“The complexity of genetic variations in the CYP2D6 gene makes it challenging to accurately predict drug response based solely on genotype or phenotype. Further research is needed to develop a more comprehensive understanding of CYP2D6 functionality, which will significantly improve our ability to optimize drug therapy.” – Dr. Jane Richards, Geneticist
This ongoing research holds great promise for the development of personalized medicine. By unraveling the intricate mechanisms of CYP2D6, scientists can identify new drug targets and pathways, leading to more effective drug discovery and development processes. Understanding how genetic variations influence drug metabolism will help researchers design medications that are tailored to individual patients’ needs, potentially reducing adverse drug reactions and improving treatment outcomes.
In addition to advancing drug discovery and development, further research on CYP2D6 will contribute to the broader field of pharmacogenomics. By elucidating the role of genetic variations in drug response, scientists can develop comprehensive guidelines and recommendations for personalized medicine. This will empower healthcare providers to deliver more targeted and effective treatments, optimizing patient care and improving overall health outcomes.
Key Challenges in CYP2D6 Research:
- The complexity of genetic variations in CYP2D6
- Predicting enzyme activity and drug metabolism accurately
- Uncovering the impact of genetic variations on drug response
- Designing targeted therapies based on CYP2D6 functionality
Overcoming these challenges will require collaboration between researchers, healthcare professionals, and pharmaceutical companies. By pooling resources and expertise, the scientific community can address these barriers and pave the way for advancements in personalized medicine.
| Advancements in CYP2D6 Research | Future Directions |
|---|---|
| Identification of new genetic variations in CYP2D6 | Investigating the functional implications of rare genetic variants |
| Development of computational models to predict CYP2D6 activity | Exploring the interaction between CYP2D6 and other drug-metabolizing enzymes |
| Integration of pharmacogenomics data into electronic health records | Conducting large-scale studies to validate CYP2D6-guided drug therapy |
Research in CYP2D6 holds significant potential for transforming drug discovery and development processes, as well as revolutionizing personalized medicine. By addressing the current challenges and delving deeper into the complexities of CYP2D6, researchers can unlock the full therapeutic potential of this crucial gene, optimizing drug therapies and improving patient outcomes.
Interesting Fact:
A recent study published in The Journal of Pharmacology and Experimental Therapeutics revealed that certain CYP2D6 genetic variations can affect the metabolism of commonly prescribed medications, leading to variable drug efficacy and potential side effects. This highlights the importance of ongoing research in understanding CYP2D6 functionality and its impact on medication response.
Integration of CYP2D6 Testing in Clinical Practice
The successful integration of CYP2D6 testing into clinical practice requires close collaboration between healthcare providers, pharmacists, and laboratory professionals. By working together, they can ensure that CYP2D6 testing is implemented effectively, leading to improved patient care.
Healthcare systems play a crucial role in this integration process. It is important for these systems to establish clear guidelines and protocols for CYP2D6 testing. These guidelines should encompass all aspects of testing, including the interpretation of results and decision-making in drug therapy. By standardizing the testing process, healthcare providers can ensure consistent and reliable outcomes.
Electronic health records (EHRs) and clinical decision support tools can play an instrumental role in facilitating the integration of CYP2D6 testing. These tools can provide healthcare providers with easy access to patients’ CYP2D6 genotype or phenotype information, enabling them to make informed decisions when prescribing medications. By leveraging technology, healthcare providers can optimize drug therapy regimens and improve patient outcomes.
Education and awareness are also vital components of integrating CYP2D6 testing. Healthcare professionals should be educated about the importance of CYP2D6 testing and its impact on personalized medicine. They should be familiar with the latest research and guidelines related to CYP2D6 testing, allowing them to make confident and evidence-based decisions. Similarly, patients should be informed about the benefits of CYP2D6 testing, empowering them to actively participate in their own healthcare.
| CYP2D6 Testing Integration Checklist | Status |
|---|---|
| Establish clear guidelines and protocols for CYP2D6 testing | ✓ |
| Implement electronic health records (EHRs) and clinical decision support tools | ✓ |
| Educate healthcare professionals about CYP2D6 testing and its clinical implications | ✓ |
| Inform and educate patients about the benefits of CYP2D6 testing | ✓ |
By following these steps, healthcare systems can successfully integrate CYP2D6 testing into clinical practice, leading to more personalized and effective patient care. Incorporating pharmacogenomics, including CYP2D6 testing, into routine clinical workflows has the potential to revolutionize drug therapy, minimize adverse drug reactions, and optimize treatment outcomes. As research in this field continues to advance, healthcare providers should stay updated and continue to explore ways to improve patient care through the integration of CYP2D6 testing.
Conclusion
The CYP2D6 gene has a critical role in drug metabolism, impacting an individual’s response to medications. By understanding a patient’s CYP2D6 phenotype, healthcare providers can make informed decisions regarding drug therapy, optimizing dosing and minimizing the risk of adverse drug reactions. Implementing CYP2D6 testing in clinical practice is a crucial step towards personalized medicine, ensuring tailored treatment plans that improve patient care.
As advancements in pharmacogenomics continue, the role of CYP2D6 in drug therapy will evolve, leading to more precise and effective treatment strategies. The study of genetic variations in CYP2D6 allows healthcare professionals to better predict patient outcomes, adjust dosing regimens, and optimize drug discovery and development processes. These advancements have the potential to revolutionize personalized medicine.
In conclusion, harnessing the power of CYP2D6 and pharmacogenomics provides a pathway to enhanced patient care. By incorporating CYP2D6 testing and understanding its impact on drug metabolism, healthcare providers can deliver tailored treatment plans, improving both efficacy and safety. As research in this field progresses, personalized medicine will continue to transform the healthcare landscape, empowering healthcare providers to optimize drug therapy and improve patient outcomes.
FAQ
What is the CYP2D6 gene and how does it metabolize?
The CYP2D6 gene is responsible for breaking down medications such as codeine and tricyclic antidepressants into active or inactive forms. It plays a crucial role in drug metabolism by converting these drugs into metabolites that can be eliminated from the body.
What is the importance of CYP2D6 in drug metabolism?
Understanding the function of CYP2D6 is important in the field of pharmacogenomics and personalized medicine. It determines how individuals respond to certain medications based on their genetic variations in the CYP2D6 gene. These genetic variations can result in different levels of enzyme activity, leading to variability in drug metabolism and medication response.
What is the role of CYP2D6 in pharmacogenetics?
CYP2D6 is a key enzyme involved in drug metabolism. Genetic variations in the CYP2D6 gene can influence an individual’s response to medications, leading to variation in drug metabolism, drug efficacy, and susceptibility to side effects. By identifying a patient’s CYP2D6 phenotype, healthcare providers can tailor drug therapy to optimize treatment outcomes and minimize the risk of adverse drug reactions.
What is the structure and function of CYP2D6?
CYP2D6 belongs to the cytochrome P450 family of enzymes and has a specific structure that allows it to bind to certain drugs and facilitate their breakdown into metabolites. Genetic and environmental factors can influence the function of CYP2D6, affecting its ability to metabolize drugs effectively.
How is the regulation and expression of CYP2D6 influenced?
The expression and activity levels of CYP2D6 can vary between individuals due to factors such as drug interactions, age, sex, disease conditions, and genetic variations. Understanding the regulation and expression of CYP2D6 is crucial for predicting drug metabolism and response in individuals.
What are the clinical implications of CYP2D6 variability?
CYP2D6 variability has significant clinical implications. Poor metabolizers, who have reduced or no enzyme activity, may require lower drug doses to avoid toxic effects. Ultra-rapid metabolizers, on the other hand, may require higher doses to achieve therapeutic effects. Adjusting drug dosing based on an individual’s CYP2D6 phenotype is important for optimizing treatment outcomes and preventing adverse drug reactions.
How is CYP2D6 testing implemented in clinical practice?
CYP2D6 testing, either through genotyping or phenotype testing, can determine an individual’s CYP2D6 activity and guide treatment decisions. It is currently recommended for certain medications with known interactions with the enzyme. Guidelines from organizations such as CPIC and DPWG provide recommendations for CYP2D6 testing and drug dosing based on genotype or phenotype.
What are the challenges and future directions in CYP2D6 research?
Despite advances in understanding the role of CYP2D6 in drug metabolism, challenges remain in accurately predicting drug response based on genotype or phenotype. The complexity and diversity of genetic variations in CYP2D6 make it difficult to accurately predict enzyme activity and drug metabolism. Further research is needed to improve our understanding of CYP2D6 functionality and its impact on drug therapy.
How is CYP2D6 testing integrated into clinical practice?
The integration of CYP2D6 testing into clinical practice requires collaboration between healthcare providers, pharmacists, and laboratory professionals. Establishing guidelines and protocols for testing, interpretation of results, and decision-making in drug therapy is crucial. Electronic health records and clinical decision support tools can aid healthcare providers in making informed decisions based on CYP2D6 genotype or phenotype.
What is the conclusion regarding CYP2D6 and drug metabolism?
The CYP2D6 gene plays a vital role in drug metabolism, and genetic variations in this gene can influence an individual’s response to medications. Understanding a patient’s CYP2D6 phenotype can guide drug therapy decisions, optimize dosing, and reduce the risk of adverse drug reactions. Implementing CYP2D6 testing in clinical practice is a crucial step toward personalized medicine and improved patient care.