Personalized Medicine Revolution: How Pharmacogenomics is Changing Treatment Plans
In the era of personalized medicine, treatment plans are no longer a one-size-fits-all approach. Pharmacogenomics, a branch of personalized medicine, is revolutionizing the way medical treatments are created and implemented. By analyzing an individual’s unique genetic profile, we see how pharmacogenomics is changing treatment plans. Pharmacogenomics allows for tailored therapy based on genetic variations that influence drug metabolism and response.

Key Takeaways in How Pharmacogenomics is Changing Treatment Plans
- Pharmacogenomics is transforming treatment plans by considering an individual’s genetic profile.
- Personalized medicine focuses on tailoring medical treatments to an individual’s unique characteristics.
- Genetic testing plays a crucial role in identifying genetic variations that influence drug metabolism.
- Targeted treatment based on pharmacogenomics can improve medication management and patient outcomes.
- The integration of pharmacogenomics into clinical practice offers new opportunities for precision medicine.
The Concept of Personalized Medicine
Personalized medicine is the practice of tailoring medical treatments to the individual characteristics of each patient, including their genetic, epigenomic, and clinical information. By considering an individual’s unique genomic profile, personalized medicine aims to enhance prediction of treatment outcomes and improve safety and efficacy. This approach goes beyond the traditional one-size-fits-all model and allows for a more proactive and preventive approach to healthcare.
Personalized medicine focuses on early disease detection through the enhanced use of biomarkers and genomic and epigenomic events. This innovative approach takes into account the specific needs of each patient, enabling healthcare professionals to develop targeted therapy plans. Tapping into the vast potential of genetic testing and technology, personalized medicine offers tailored therapy options that can revolutionize treatment plans and patient care.
Advantages of Personalized Medicine:
- Increased treatment efficacy
- Minimized adverse reactions
- Better patient outcomes
- Optimized medication management
- Proactive and preventive healthcare
“Personalized medicine is a game-changer in the world of healthcare. By tailoring treatment plans to the unique genetic profiles of individuals, we can unlock new possibilities and vastly improve patient outcomes.”
The integration of personalized medicine into healthcare systems can potentially reduce costs by avoiding unnecessary and ineffective treatments. By leveraging genetic and clinical data, healthcare professionals can make more informed decisions about drug selection, dosage, and potential side effects. This approach not only enhances patient care but also paves the way for advancements in targeted therapies and precision medicine.
| Personalized Medicine | Traditional Medicine |
|---|---|
| Patient-centric approach | One-size-fits-all model |
| Enhanced treatment outcomes | Generalized treatment efficacy |
| Minimized adverse drug reactions | Potential for adverse reactions |
| Improved medication management | Limited individualization |
The Power of Pharmacogenomics
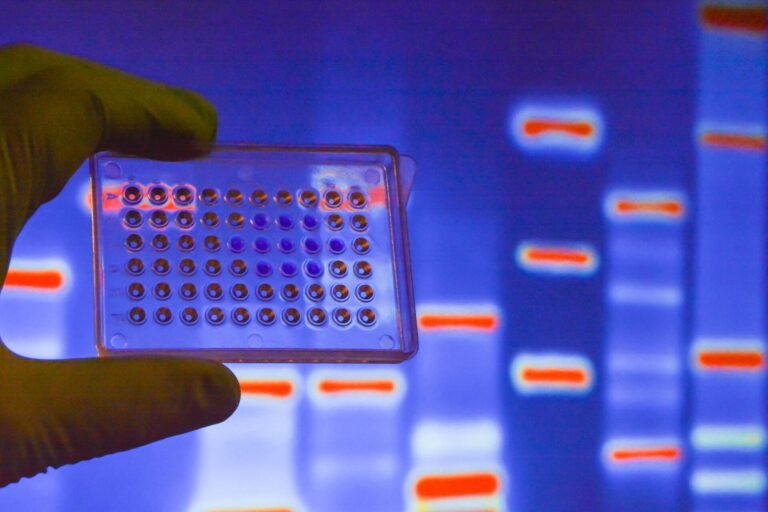
Pharmacogenomics, a branch of personalized medicine, explores how an individual’s genetic makeup influences their response to drugs. By analyzing genetic markers, such as specific variations in genes responsible for drug metabolism, healthcare professionals can gain valuable insights into a patient’s potential response to a particular medication. This knowledge allows for a more personalized approach to drug therapy and enables healthcare professionals to make informed decisions about drug selection, dosage, and potential side effects.
Pharmacogenomics has the potential to significantly improve treatment outcomes. By tailoring drug therapy based on an individual’s genetic markers, healthcare providers can optimize drug efficacy and minimize adverse reactions. This approach not only enhances patient well-being but also leads to more efficient and targeted medication management.
“The ability to analyze genetic markers related to drug response is a game-changer in pharmacology. It allows us to take into account individual genetic variations and tailor treatment plans accordingly. This personalized approach has the potential to revolutionize drug therapy.” – Dr. Elizabeth Collins, Pharmacologist
Furthermore, pharmacogenomics has transformative implications for drug development and approval processes. By identifying patient subgroups that are most likely to benefit from specific medications, pharmacogenomics can expedite the development of targeted medications and streamline the regulatory approval process.
The Role of Genetic Markers
Genetic markers play a fundamental role in pharmacogenomics. These markers are specific variations in genes that can influence how a patient responds to a particular drug. By identifying these markers through genetic testing, healthcare professionals can gain critical insights into a patient’s drug response profile.
For example, genetic markers can provide information about a patient’s likelihood of experiencing adverse drug reactions or their metabolism of specific medications. Armed with this knowledge, healthcare professionals can adjust drug dosage, select alternative medications, or monitor patients more closely to ensure optimal treatment outcomes.
Improving Patient Care with Pharmacogenomics
Pharmacogenomics offers significant benefits in terms of patient care. By harnessing the power of genetic markers, healthcare professionals can:
- Personalize drug therapy to improve treatment outcomes
- Minimize adverse drug reactions and side effects
- Optimize drug efficacy and dosage
- Enhance medication management and adherence
This personalized approach to drug therapy is particularly valuable for patients with chronic conditions who may require long-term medication. By tailoring treatment plans to an individual’s genetic profile, healthcare professionals can provide targeted and effective therapies, ultimately improving patient satisfaction and quality of life.
Examples of Genetic Markers and Drug Responses
| Genetic Marker | Drug Response |
|---|---|
| CYP2C19*2 | Reduced drug metabolism, increased risk of adverse effects |
| DPYD*2A | Increased risk of severe toxicity with certain chemotherapy drugs |
| SLCO1B1 | Reduced drug uptake, altered effectiveness of statin therapy |
Challenges and Opportunities in Implementing Pharmacogenomics
The implementation of pharmacogenomics poses various challenges in the field of healthcare. These challengesencompass scientific, economic, operational, and policy-related aspects, which necessitate careful consideration and planning. One of the primary challenges is the development of new diagnostic techniques to stratify patients at a higher resolution and optimize therapeutic selection and timing. By enhancing diagnostic techniques, healthcare professionals can provide more precise and effective treatments tailored to individual patients’ genetic profiles.
Another critical aspect in the successful integration of pharmacogenomics into clinical practice is education and training for healthcare professionals, including physicians, genetic counselors, and pharmacists. It is essential to equip these professionals with the knowledge and skills required to interpret and utilize genetic information effectively in the context of patient care. By investing in education, healthcare professionals can confidently implement pharmacogenomic strategies and contribute to improved patient outcomes.
Collaboration between pharmaceutical companies and academic research teams is pivotal in driving innovation and the development of new technologies in pharmacogenomics. By combining their expertise and resources, these collaborations can accelerate advancements in diagnostic tools, therapeutic approaches, and precision medicine. Such partnerships can lead to the discovery of novel drug targets, the development of more effective medications, and the refinement of diagnostic techniques, ultimately benefiting patients on a broader scale.
Additionally, the protection of private information and coordination between government research and regulatory agencies are vital considerations in the implementation of pharmacogenomics. Ensuring the privacy and security of patients’ genetic data is crucial to maintain trust in the healthcare system. Furthermore, effective communication and collaboration between research and regulatory entities are necessary to establish guidelines and regulations that support the safe and ethical use of pharmacogenomic information in clinical practice.
Challenges and Opportunities in Implementing Pharmacogenomics Summary Table
| Challenges | Opportunities |
|---|---|
| Scientific challenges in developing diagnostic techniques for precise patient stratification. | Collaboration between pharmaceutical companies and academic research teams to drive innovation. |
| Economic challenges in funding research and development of new technologies. | Education and training for healthcare professionals to effectively utilize pharmacogenomic information. |
| Operational challenges in integrating pharmacogenomics into clinical practice. | Protection of private information and coordination between government research and regulatory agencies. |
| Policy-related challenges in establishing guidelines and regulations for the use of pharmacogenomics. |
The Role of Education in Pharmacogenomics
The field of pharmacogenomics relies heavily on education and training to ensure that healthcare professionals possess the knowledge and skills necessary to effectively utilize genetic information in personalized medicine. As the intersection of pharmacology and genomics, pharmacogenomics plays a crucial role in tailoring treatment plans to individual patients based on their unique genetic profiles.
Genetic counselors are key players in the education process, providing valuable guidance and counseling to both patients and healthcare professionals. They play a vital role in explaining the benefits and implications of pharmacogenomic testing, helping individuals understand how their genetic makeup influences drug response and treatment outcomes.
Continuing education is essential in the rapidly evolving field of pharmacogenomics. Healthcare professionals must stay updated with the latest research and developments to ensure they can effectively implement and interpret pharmacogenomic information in their clinical practice. This includes learning about advancements in genetic testing technologies, understanding the significance of genetic variations in drug metabolism, and staying informed about the most recent medical interventions and treatment approaches.
Collaboration and interdisciplinary education programs, such as interprofessional education, can greatly enhance the understanding and implementation of pharmacogenomics in clinical practice. By fostering collaboration among healthcare professionals from different disciplines, these programs promote a deeper understanding of the role of pharmacogenomics in personalized medicine and facilitate more comprehensive patient care.
Benefits of Education in Pharmacogenomics
| Benefits | Description |
|---|---|
| Optimized treatment selection and dosage | Educated healthcare professionals can make informed decisions based on pharmacogenomic information, leading to more precise and effective treatment plans. |
| Reduced adverse drug reactions | Understanding genetic variations can help healthcare professionals identify patients at higher risk of adverse drug reactions and make necessary adjustments to medication management. |
| Enhanced therapeutic outcomes | Applying pharmacogenomic knowledge can lead to improved treatment outcomes, as individual patients receive tailored therapies based on their genetic profiles. |
| Increased patient satisfaction | Education in pharmacogenomics empowers healthcare professionals to provide personalized care, enhancing patient satisfaction and engagement in their treatment plan. |

Education plays a crucial role in harnessing the potential of pharmacogenomics and ensuring that healthcare professionals are equipped to provide personalized care to their patients. By staying informed, collaborating across disciplines, and integrating the latest research and developments, healthcare professionals can optimize treatment outcomes and revolutionize healthcare through the power of pharmacogenomics.
Public Perception and Adoption of Pharmacogenomics
Public attitudes play a crucial role in the widespread adoption of pharmacogenomics in healthcare. Studies have shown that there is a need for increased public awareness and understanding of pharmacogenetic testing and its potential benefits. When individuals are educated about the value of pharmacogenomics, they are more likely to embrace this personalized approach to healthcare.
Physicians’ beliefs and attitudes towards pharmacogenomics also have a significant impact on its adoption and integration into clinical practice. It is important for healthcare providers to recognize the potential of pharmacogenetic testing in improving treatment outcomes and minimizing adverse drug reactions. By incorporating pharmacogenomic information into their decision-making process, physicians can ensure that patients receive tailored therapies that maximize efficacy and minimize risks.
Genetic counseling plays a vital role in bridging the gap between patients and healthcare professionals in understanding and utilizing pharmacogenomic information. Genetic counselors are trained to provide guidance and support to individuals seeking genetic testing. They can help patients navigate the complexities of genetic information, interpret test results, and make informed decisions about their healthcare.
Genetic counseling is a collaborative process that empowers individuals to make informed choices about their health based on their genetic profiles. By working alongside healthcare professionals, genetic counselors facilitate the integration of pharmacogenomics into clinical practice.
The Future of Pharmacogenomics
The field of pharmacogenomics is constantly evolving, driven by advancements in genetic testing and technology. These continuous developments hold great promise for the future of personalized medicine and the optimization of treatment plans.
One significant area of progress is in the use of liquid biopsies. These tests have the potential to detect genetic mutations and diseases at an early stage, enabling early intervention and the customization of treatment plans. Liquid biopsies provide a non-invasive and efficient means of monitoring genetic variations, further enhancing the implementation of pharmacogenomics in clinical practice.
An exciting breakthrough in the field of pharmacogenomics is the advent of CRISPR-Cas9 technology. This powerful gene-editing tool allows for precise modifications to an individual’s genetic makeup. With CRISPR-Cas9, researchers and healthcare professionals can potentially create treatments that are tailored to each patient’s unique genetic profile, leading to more effective interventions and improved health outcomes.
Looking ahead, pharmaceutical companies will play a crucial role in advancing pharmacogenomics by investing in the development of new diagnostic techniques and technologies. By harnessing the potential of genetic testing and technology advancements, medical interventions can be further refined and optimized to address individual patient needs.
The future of pharmacogenomics holds great promise for revolutionizing healthcare by providing individualized, targeted therapies and improving patient outcomes. As research continues and technology advances, personalized medicine will become increasingly accessible, offering new possibilities for precision healthcare.
Implementing Pharmacogenomics in Clinical Practice
Clinical implementation of pharmacogenomics involves the utilization of diagnostic tools and advanced technologies to accurately identify genetic variations and predict individual drug responses. By leveraging these tools, healthcare professionals can make informed treatment decisions based on pharmacogenomic information, leading to better patient outcomes and personalized therapy.
The Role of Diagnostic Tools
Diagnostic tools play a crucial role in the clinical implementation of pharmacogenomics. These tools enable the identification of specific genetic markers, such as single nucleotide polymorphisms (SNPs), that are associated with drug metabolism and response. By analyzing these markers, healthcare professionals can tailor treatment plans to each patient’s unique genetic profile, enhancing the effectiveness and safety of drug therapies.
Clinical Decision Support Systems
Another important aspect of implementing pharmacogenomics in clinical practice is the use of clinical decision support systems (CDSS). These computer-based tools provide healthcare professionals with evidence-based recommendations and guidelines for drug selection, dosage adjustments, and monitoring based on an individual’s pharmacogenomic profile.
“CDSS can integrate patient-specific genetic information with drug databases, clinical guidelines, and patient electronic health records to provide real-time, personalized treatment recommendations.”
The integration of CDSS into electronic health record systems can streamline the clinical decision-making process, improving efficiency and ensuring that healthcare professionals have access to up-to-date and relevant pharmacogenomic information.
Pre-Emptive Genotyping
Pre-emptive genotyping involves conducting genetic testing before drug prescription to identify potential drug-gene interactions and optimize drug selection and dosage for individual patients. By proactively genotyping patients, healthcare professionals can anticipate potential adverse drug reactions, select the most appropriate medications, and adjust dosages based on predicted response patterns.
This pre-emptive approach to genotyping empowers healthcare professionals to personalize treatment plans from the outset, reducing the trial-and-error process commonly associated with medication management.
Integrating Pharmacogenomic Testing
In order to ensure the widespread use of pharmacogenomics in clinical practice, it is crucial to integrate pharmacogenomic testing into clinical practice guidelines and include this information in drug labels. By incorporating pharmacogenomic testing recommendations into guidelines and labeling, healthcare professionals will be encouraged to utilize this valuable information in their decision-making process, ultimately leading to improved patient care and medication management.
Table: The Benefits of Implementing Pharmacogenomics in Clinical Practice
| Benefits | Explanation |
|---|---|
| Personalized Treatment | Consideration of an individual’s genetic profile allows for customized therapy that is tailored to their unique needs and characteristics. |
| Improved Treatment Outcomes | By optimizing drug selection and dosages based on genetic information, treatment efficacy can be enhanced, resulting in improved patient outcomes. |
| Reduced Adverse Drug Reactions | Identification of potential drug-gene interactions can help mitigate the risk of adverse reactions and minimize harm to patients. |
| Enhanced Medication Management | Integration of pharmacogenomic information into clinical practice allows for more precise medication management, reducing the need for trial-and-error approaches. |
Conclusion
In conclusion, pharmacogenomics is transforming treatment plans by customizing therapy based on individual genetic profiles. This branch of personalized medicine holds great promise for targeted treatment, improved medication management, and better patient outcomes. By analyzing genetic variations that influence drug metabolism and response, healthcare professionals can make informed decisions about drug selection, dosage, and potential side effects.
Despite its potential, there are challenges that need to be addressed for pharmacogenomics to fully realize its benefits. Education and implementation are key areas that require attention to ensure healthcare professionals are adequately trained and equipped to utilize genetic information for personalized medicine. Additionally, collaboration between industry stakeholders and regulatory agencies is essential for driving innovation, developing new diagnostic techniques, and advancing technology in the field.
As genetic testing and technology continue to advance, the future of pharmacogenomics looks promising. The integration of pharmacogenomic information into clinical practice guidelines and drug labels can further enhance its widespread use. With further research, advancements, and effective implementation, pharmacogenomics has the potential to revolutionize treatment plans and improve patient outcomes, paving the way for truly personalized and precise healthcare.
FAQ
What is pharmacogenomics?
Pharmacogenomics is the study of how an individual’s genetic makeup affects their response to drugs. It involves analyzing genetic markers that influence drug metabolism and response to predict how a patient will respond to a particular medication.
How does pharmacogenomics change treatment plans?
Pharmacogenomics revolutionizes treatment plans by tailoring therapy to an individual’s unique genetic profile. By considering genetic variations that affect drug metabolism, healthcare professionals can make more informed decisions about drug selection, dosage, and potential side effects.
What are the benefits of personalized medicine?
Personalized medicine, driven by pharmacogenomics, offers targeted treatment, improved medication management, and better patient outcomes. It shifts the focus from a one-size-fits-all approach to an individualized therapy approach, leading to more effective treatments and minimized adverse drug reactions.
What are the challenges in implementing pharmacogenomics?
The implementation of pharmacogenomics faces challenges such as scientific, economic, operational, and policy-related issues. This includes the development of new diagnostic techniques, education and training of healthcare professionals, collaboration between stakeholders, and protection of private information.
What is the role of education in pharmacogenomics?
Education plays a crucial role in the successful integration of pharmacogenomics into clinical practice. Healthcare professionals, including physicians, genetic counselors, and pharmacists, need to be educated and trained in utilizing genetic information for personalized medicine.
How do public attitudes and physician beliefs impact the adoption of pharmacogenomics?
Public attitudes towards pharmacogenetic testing and physicians’ beliefs influence the widespread adoption of pharmacogenomics in healthcare. Increased public awareness and understanding, as well as effective communication between patients and healthcare professionals, are crucial in promoting the benefits and implications of pharmacogenomic testing.
What does the future of pharmacogenomics look like?
The field of pharmacogenomics is constantly evolving with advancements in genetic testing and technology. New developments, such as liquid biopsies and gene editing technologies, hold promise for early disease detection and personalized treatments based on individual patients’ genetic makeup.
How can pharmacogenomics be implemented in clinical practice?
Clinical implementation of pharmacogenomics requires the use of diagnostic tools and technologies to accurately identify genetic variations and predict drug response. Clinical decision support systems and pre-emptive genotypingcan assist healthcare professionals in making informed treatment decisions based on pharmacogenomic information.
What is the conclusion about pharmacogenomics?
Pharmacogenomics is revolutionizing treatment plans by tailoring therapy to individual genetic profiles. It offers the potential for targeted treatment, improved medication management, and better patient outcomes. However, challenges such as education and implementation need to be addressed for pharmacogenomics to reach its full potential.
Source Links
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5492710/
- https://www.mayo.edu/research/centers-programs/center-individualized-medicine/about/video-center
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5391796/